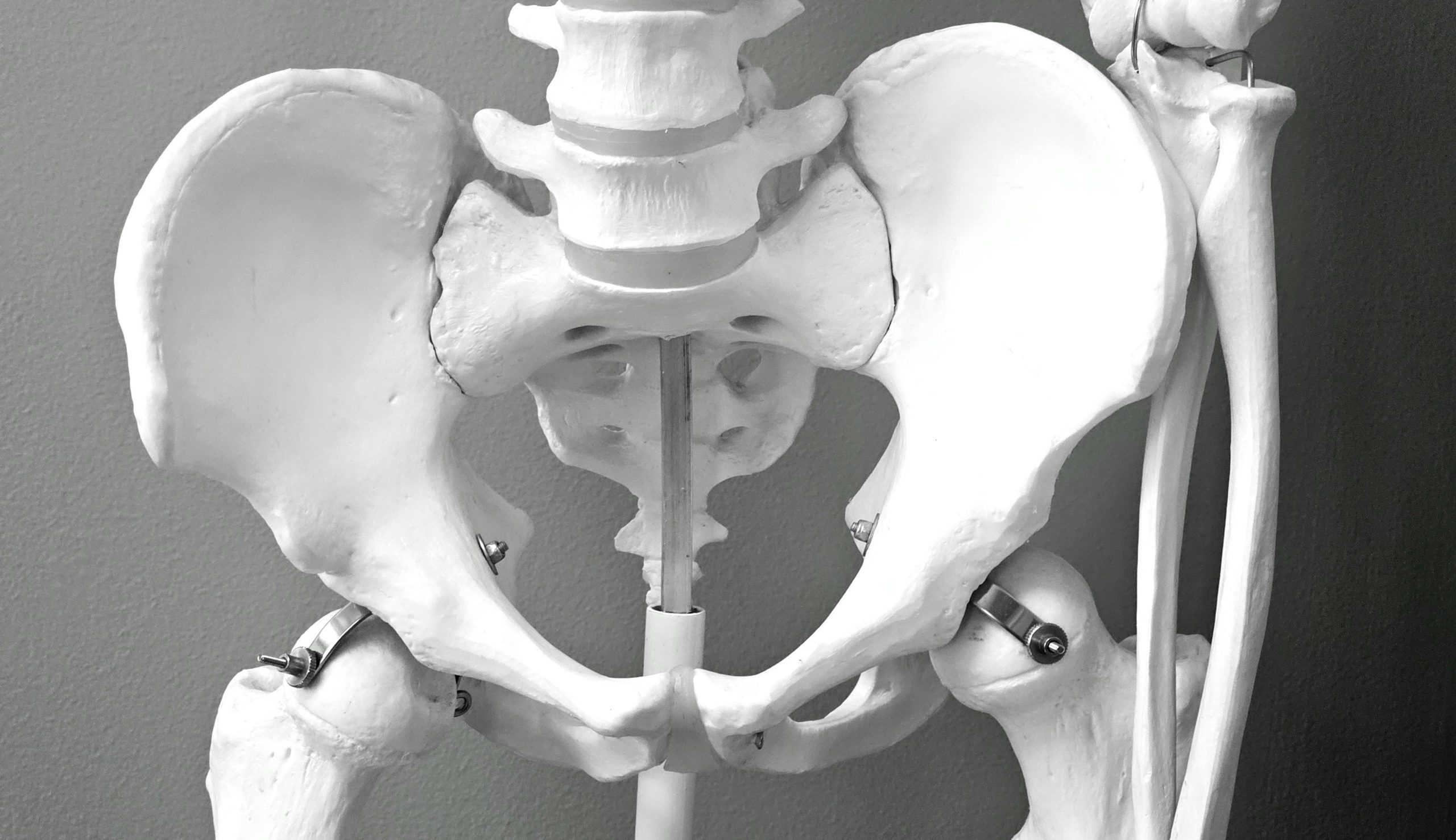
When you think about preventative health you often think about diabetes, cholesterol, heart disease and cancer, but how often do you think about your bones? Osteoporosis is a condition of low bone density or weaker bones. This increases the risk of breaking a bone, even with minor falls. Having a fracture, especially of a major bone, like the hip or pelvis, can lead to reduced quality of life due to pain issues, limited mobility and loss of independence. It’s therefore very important to try and prevent osteoporosis or reduce the extent of it as soon as possible.
Risk factors:
Older age, especially being over 70, having a previous fracture, especially after a minor incident, and having a parent with a hip fracture are big risk factors for osteoporosis. Some other risk factors include the following:1,2
- Lifestyle factors
- Low calcium intake
- Low Vitamin D
- Low muscle mass and/or low body weight
- Smoking
- Alcohol >2 standard drinks/day
- Medical Conditions
- Coeliac disease
- Conditions affecting the thyroid or parathyroid glands
- Diabetes
- Rheumatoid Arthritis
- Early menopause/low testosterone
- Chronic liver disease or chronic kidney disease
- Organ transplant
- HIV
- Myeloma
- Medications
- Regular use of steroid medications such as prednisolone
- Some medications used to treat breast or prostate cancer (sometimes used for endometriosis treatment as well)
- Some anti-epileptic treatments (some of these may also be used for treatment of mental health conditions)
- Maintain an adequate daily calcium intake throughout your life
Calcium needs differ across the lifespan. Men 19-70 years old and women from 19-50 need 1000 mg of calcium per day, and women over 50 and men over 70 require 1300 mg per day.2 Ideally this is obtained through your diet by eating calcium rich foods.
This handout from Healthy Bones Australia lists the calcium content of common foods so you can work out your average daily intake.3 If you’re not able to achieve the recommended amount in your diet, it’s best to consult a doctor to discuss the need for supplements. - Maintaining adequate Vitamin D levels
Vitamin D helps your intestines absorb enough calcium from your diet. It also helps regulate calcium levels in the blood and supports skeletal growth.4 Vitamin D is present in some foods such as egg yolks, liver, oily fish and some products specifically fortified with vitamin D but consuming these aren’t enough to reach adequate levels in the blood.4
The biggest source of Vitamin D is through exposure to sunlight. In Australia, there is a delicate balance of low sunlight exposure leading to low vitamin D and higher sunlight exposure that increases the risk of skin cancer. Additionally, people with darker skin, those who spend most of their time indoors or those who cover most of their body when outside are at higher risk of vitamin D deficiency. Patients at risk of low vitamin D, or those that have been diagnosed with low bone density should talk to their doctor about having their vitamin D levels tested as they may need supplements. - Specific exercises to prevent osteoporosis5
Weight bearing exercise: You can strengthen your bones by using your bodyweight to work the bones that support you. Options include jogging, jumping, skipping, step ups, dancing or sports with running or quick changes in direction.
Resistance exercise: It is important to improve muscle strength around the bones prone to fracture. Exercises should target the major muscle groups in the arms, legs and spine and can include yoga, pilates or weights.
Balance exercise: Improving balance reduces your risk of falls and, therefore, fractures. This can be done through formal practices such as Tai Chi, or simple exercises at home that improve your standing balance, and your ability to manoeuvre around obstacles on the ground.
You can read more about exercise options at Healthy Bones Australia, but if you are new to these exercises, you have other health conditions, or you have already been diagnosed with osteoporosis, it is best to get individualised recommendations from a doctor, physiotherapist or an exercise physiologist.4 - Getting tested for osteoporosis
If you have any of the risk factors listed above, or you are concerned about osteoporosis, it’s best to chat to your GP about when is best to get a bone density scan (DEXA) to check if you have osteoporosis.
Osteoporosis is a condition that can significantly impact your quality of life. Making changes to your diet and exercise routine can delay the onset of osteoporosis and help you avoid fractures and their complications.
References:
- The Royal Australian College of General Practitioners (RACGP), Healthy Bones Australia. Osteoporosis management and fracture prevention in postmenopausal women and men over 50 years of age, 3rd edition. RACGP, 2024.
- Healthy Bones Australia. Breaking a Bone and Bone Health [Internet]. Healthy Bones Australia. 2023. Available from: https://healthybonesaustralia.org.au/resource-hub/fact-sheets/breaking-bone/
- Healthy Bones Australia. Calcium Content of Common Foods [Internet]. Healthy Bones Australia. 2022. Available from: https://healthybonesaustralia.org.au/wp-content/uploads/2022/10/calcium-rich-food-list_en_1_healthybonesaustralia-iof-version-draft-1.pdf
- Healthy Bones Australia. Exercise & Bone Health – Bone Health [Internet]. Healthy Bones Australia. Available from: https://healthybonesaustralia.org.au/your-bone-health/exercise-bone-health/